Abstract
Introduction Myelodysplastic/myeloproliferative (MDS/MPN) overlap syndromes (MDS/MPN) are rare disorders characterized by concomitant myeloid hyperplasia and dysplasia. Only recognized as distinct disorders since 2001, this heterogeneous group includes chronic myelomonocytic leukemia (CMML), MDS/MPN with ringed sideroblasts and thrombocytosis (MDS/MPN-RS-T), atypical chronic myeloid leukemia (aCML), juvenile myelomonocytic leukemia (JMML) and MDS/MPN-unclassifiable (MDS/MPN-U). Timely and accurate diagnosis can be difficult outside academic medical centers, and epidemiological data are lacking. This study aims to evaluate national survival outcomes, population and disease characteristics, and socioeconomic and demographic features associated with disparate survival in these rare and complex disorders.
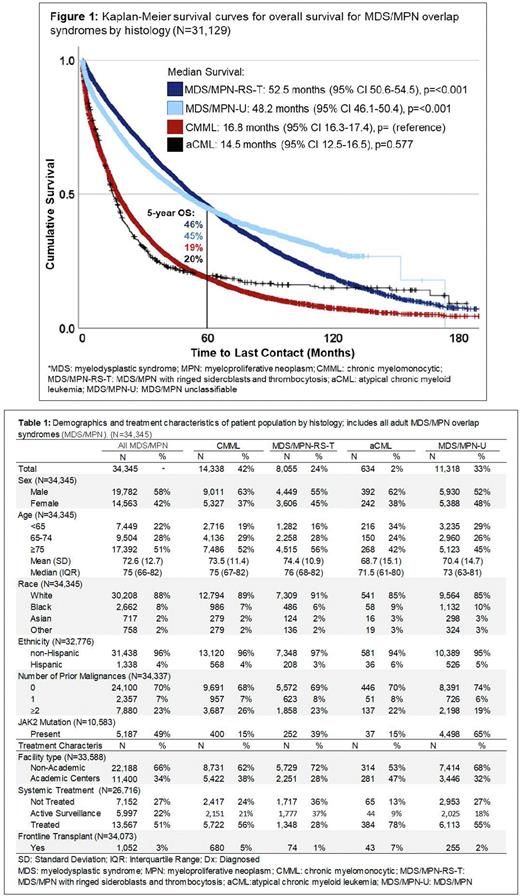
Methods Utilizing the National Cancer Database from 2004-2019, MDS/MPN was identified by histology codes for aCML (9876), CMML (9945), MDS/MPN-U (9975), and MDS/MPN-RS-T (9982). Only adult (age >18) patients (pts) were included, excluding JMML. Demographic, socioeconomic, and first line treatment characteristics were identified for all MDS/MPN and by histology. Kaplan-Meier survival analysis was used to compare overall survival (OS), with multivariable Cox regression, adjusted for age, sex, race, ethnicity, Charlson-Deyo comorbidity score, treatment facility type, and insurance to evaluate features associated with disparate survival outcomes.
Results Of the 34,245 MDS/MPN pts identified, 42% (N=14,338) had CMML, 24% (N=8,055) had MDS/MPN-RS-T, 2% (N=634) had aCML, and 33% (N=11,318) were diagnosed with MDS/MPN-U. The median age at diagnosis was 75 years (yrs) (interquartile range 66-82). MDS/MPN-RS-T and aCML pts presented at the oldest and youngest ages (median 76 yrs vs 71 yrs). The majority of pts were male (58%), and White (88%; 8% Black and 2% Asian). Notably, aCML and MDS/MPN-U pts were more likely to be a race other than White (both 15% non-White), compared to CMML (11%) and MDS/MPN-RS-T (9%), p<0.001. While molecular data is limited in the NCDB, of the 10,583 cases with JAK2 testing reported, 49% had a JAK2 mutation. This was greatest in the MDS/MPN-U group, at 65% of pts, followed by 39% of MDS/MPN-RS-T pts, and15% for both aCML and CMML pts.
Approximately half of MDS/MPN pts (51%) received disease directed therapy at diagnosis, with 22% managed with active surveillance, and 27% not receiving treatment, for reasons including early death, contraindication, or hospice care. aCML pts were the most likely to be placed on disease directed therapy (78%), followed by CMML (56%), MDS/MPN-U (55%), and MDS/MPN-RS-T (28%).
The median OS for all MDS/MPN was 31.4 months (mos) (95% confidence interval [CI] 30.7-32.1), with a 1-, 5-, and 10-year OS of 71%, 33%, and 16%, respectively. MDS/MPN-RS-T pts had a median OS of 52.5 mos (95% CI 50.6-54.3), similar to MDS/MPN-U with a median OS of 48.2 mos (95% CI 46.1-50.4). CMML and aCML had significantly worse survival with a median OS of 16.8 mos (95% CI 16.3-17.4) and 14.5 mos (95% CI 12.5-16.5), respectively, p<0.001. On multivariable Cox regression, MDS/MPN-RS-T and MDS/MPN-U retained a significant survival advantage over CMML (Hazard ratio [HR] 0.45 [95% CI 0.43-0.46], p<0.001 and HR 0.51 [95% CI 0.49-0.53], p<0.001, respectively). However, aCML had a significantly worse survival, with HR 1.27 (95% CI 1.15-1.40, p<0.001). Age, increasing comorbidity burden, and Black race were associated with reduced survival outcomes, while female sex, private insurance, and treatment at academic centers was associated with significantly improved OS.
Conclusion We present the largest study to date on the real-world survival and demographic characteristics of MDS/MPN. Compared to prior data, which was generally limited in size, we found a lower median OS than previously reported, though MDS/MPN-U had a greater OS than prior estimates. We further identified a higher portion of MDS/MPN pts identified as MDS/MPN-U than previously estimated, and significantly higher rates of JAK2 mutations than previously reported. This study also adds clarity to ages of diagnosis, sex ratios, and racial and ethnic characteristics. We also note survival disparities in Black pts, and those who are underinsured or treated at non-academic centers, indicating that access to treatment remains a significant barrier to survival in these pts.
Disclosures
Tantravahi:Karyopharm Therapeutics Inc., Novartis, AbbVie, Incyte: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Karyopharm Therapeutics Inc.,: Research Funding. Patel:Stemline: Research Funding; Genentech/Roche: Research Funding; Incyte: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.